

Researchers say that between 1995 and 2023, the number of under-15s diagnosed with type 2 diabetes rose by about 8.3 per cent a year, with the sharpest increases among Pacific and Māori children.
Photo/University of Sydney
'Our kids are getting sick too soon': Experts warn of diabetes crisis crossing generations
A growing number of Māori and Pasifika children in Aotearoa are being diagnosed with type 2 diabetes, a disease once seen only in adults.



Inked across lands: How Pacific tattoo art is thriving in Germany
US funding cuts threaten to 'dry up' future of Pacific scientists - expert



Inked across lands: How Pacific tattoo art is thriving in Germany
US funding cuts threaten to 'dry up' future of Pacific scientists - expert
New Zealand’s health system is heading towards a crisis that Pacific health leaders warn is already unfolding in their communities - an alarming rise in type 2 diabetes among Pacific and Māori youth that’s reshaping what used to be considered an adult disease.
Experts warn this surge is a medical issue, and a social and cultural emergency that threatens to deepen long-standing inequities unless the country acts fast.
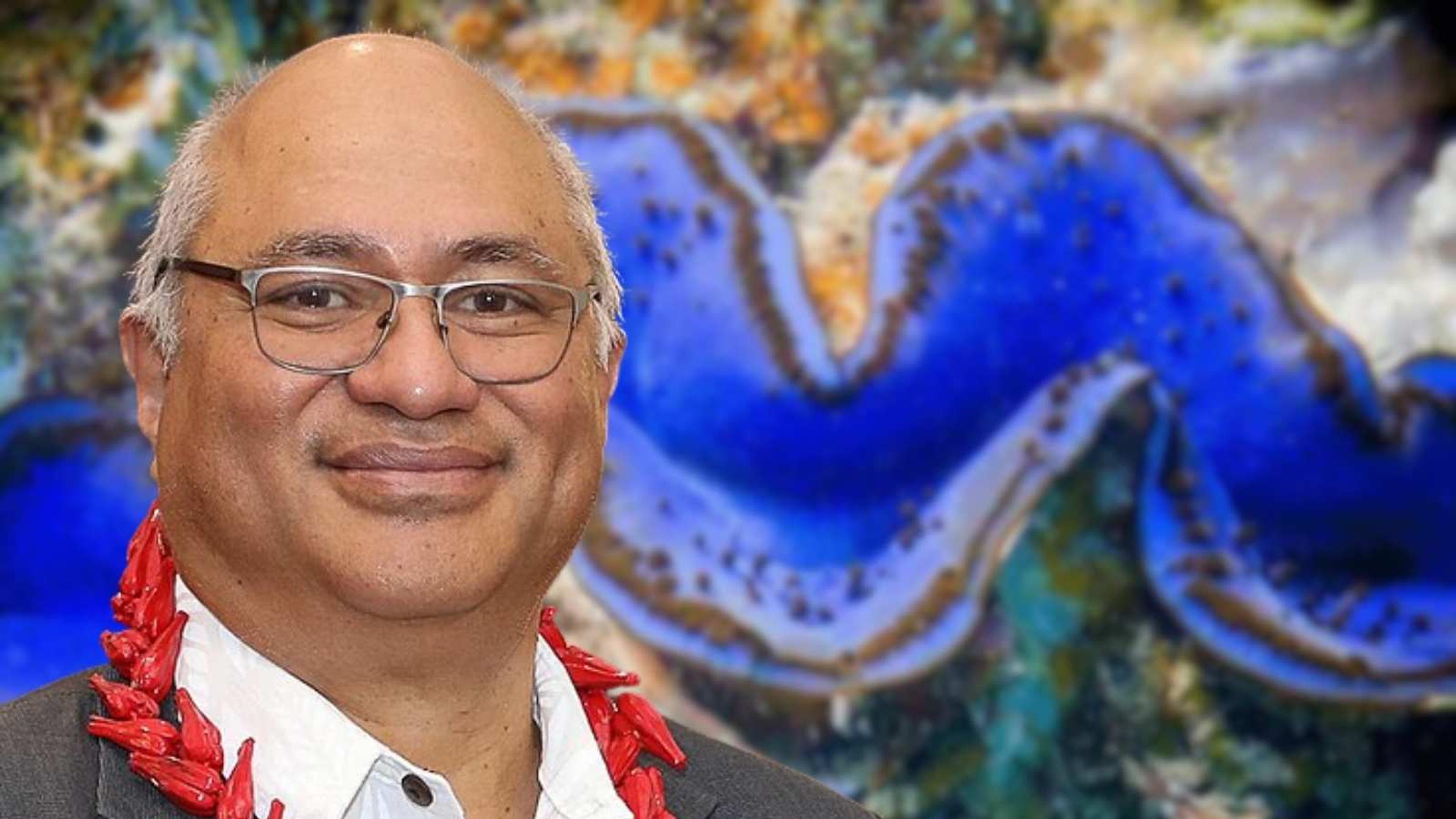
Auckland researchers say that between 1995 and 2023, the number of under-15s diagnosed with type 2 diabetes rose by about 8.3 per cent a year, with the sharpest increases among Pacific and Māori children.
In 2023, rates for Pasifika youth reached 9.84 per 100,000, more than 20 times higher than for Pākehā.
Dr Craig Jefferies, a paediatric endocrinologist at Starship Children’s Hospital, says what was “almost unheard of” is now “an everyday reality in clinics”.
“When a young person gets type 2 diabetes, the clock starts ticking on complications,” Jefferies says in a statement.
“They develop kidney failure, blindness, amputations, and heart disease decades earlier than their parents. If left undiagnosed and unsupported, the outcomes can be devastating.”
He says Pacific families are particularly affected because of intergenerational exposure, where children born to mothers with diabetes, especially during pregnancy, have a far higher lifetime risk.
“As more mothers with type 2 diabetes are having children, those children are now at higher risk. Combined with genetic predisposition, this is fuelling the growing trend in New Zealand.”

Team Cook Islands working on their project during the 2019 WAKE UP Workshop. Photo/Pacific Community/File
Why the alarm now?
Pacific health experts describe it as a “crisis of inheritance” - a disease pattern being passed from one generation to the next, intensified by systemic inequality.
Dr Viliami Tupou, a Tongan endocrinologist working in South Auckland, earlier raised the issue, saying it goes far beyond diet or lifestyle.
“This is not just about fizzy drinks or fast food,” he says. “It’s about poverty, housing, stress, and a health system that doesn’t always speak our language.
"The kids in my clinic are growing up in environments that make health almost impossible to protect.”
A 2025 New Zealand Medical Journal review found that 84.5 per cent of under-25s diagnosed with type 2 diabetes were obese, 92.8 per cent were aged 15 to 24, and most came from areas of high deprivation.
Young patients are also struggling to meet glucose-control targets: fewer than one-in-four reach healthy HbA1c levels, which means they are heading toward early complications.
Photo/BpacNZ/Tonga Health
A system not built for Pacific youth
Dr Bryan Betty, chair of General Practice New Zealand, says the health system has been slow to recognise this shift.
“For years, type 2 diabetes in young people wasn’t even on the radar for GPs. Now it must be," he says. "When a teenager shows thirst, exhaustion or rapid weight change, diabetes has to be part of the diagnostic thinking.”
But frontline doctors say the system still lacks culturally appropriate support. Pacific clinicians report that around 70 to 80 per cent of diabetes resources are adult-focused and culturally tone-deaf, and full of Western food references and medical jargon.
Dr Leilani Faumuina, a Sāmoan GP in Porirua, also says Pacific families need education that feels like it was “written for them, not at them".
“If we want Pacific kids to manage diabetes, the advice has to come in the language of love, faith and family," she says. "It has to be grounded in whānau, in aiga, in village, not shame.”
The unseen cost and silent pipeline
What hasn’t been widely discussed, experts say, is how the rise in youth type 2 diabetes creates a “silent pipeline” of future illness - of young people who will carry chronic disease into middle age, undermining national health progress.
Dr Lynne Chepulis, a researcher at the University of Waikato, warns: “We’re seeing complications in people still in their 30s and 40s - kidney disease, amputations, heart attacks - all from diabetes that began in adolescence.”
This means the country’s health, education, and social systems are already facing decades of downstream impacts - higher costs, lost productivity, and widening inequity.
A Pacific call to action
For Heather Verry, Diabetes New Zealand chief executive, the numbers are a wake-up call.
“There are around 6000 young New Zealanders under 25 living with diabetes, mostly type 1, but type 2 is rising fast," she says. "Globally, this is one of the fastest-growing health issues for young people, and our Pacific communities are at the front line.”
Verry says urgent government investment is needed to create youth-specific, culturally relevant programmes.
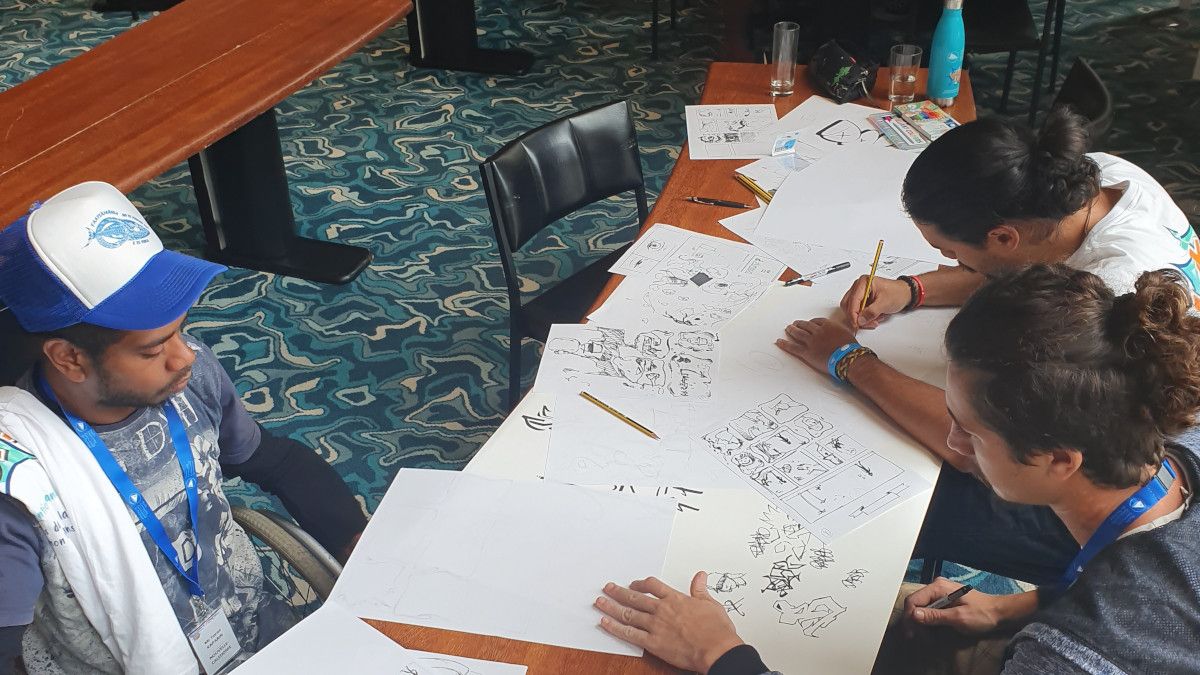
Team New Caledonia working on their project during the 2019 WAKE UP Workshop. Photo/Pacific Community/File
“There are no tailored resources for young people with type 2 diabetes, none," Verry says. "We need education that’s practical, age-appropriate and non-judgemental, that tackles mental health and stigma. These children deserve to thrive.”
Tupou adds that Pacific leadership must be central to the solution.
“Too often programmes are designed for Pacific people, not with them.
We have the expertise, the cultural knowledge, and the trust of our communities. We just need to be resourced to lead.”
What needs to happen now
Screen high-risk youth early, especially Māori, Pacific, and children of diabetic mothers.
Design Pacific-led education programmes, using church networks, village groups, and schools to spread awareness.
Fund culturally competent healthcare teams: Pacific nurses, dietitians, and community navigators in primary care.
Tackle root causes: poverty, food insecurity, poor housing and limited green space.
Invest in long-term data collection to distinguish between type 1 and type 2 diabetes in youth for clearer policy responses.
'We can’t wait until it’s everyone’s problem'
The surge in type 2 diabetes among young Pacific people, experts say, is a health statistic and a test of how seriously New Zealand treats equity.
“Nothing good comes with that increase - not for our children, our whānau, or our nation,” Jefferies says. “Unless we act now, the cost will be staggering, in lives and in resources.”
Faumuina puts it more simply: “Our kids are getting sick too soon. They deserve better food, better housing, better futures. If we change nothing, we’re condemning the next generation to a lifetime of illness before they even reach adulthood.”
For Pacific communities, the message is clear: this is not just a medical issue, it’s a call to protect the next generation, before diabetes becomes their inheritance.
For more information about Diabetes Action Month and diabetes and youth, visit www.diabetesactionmonth.org.nz