

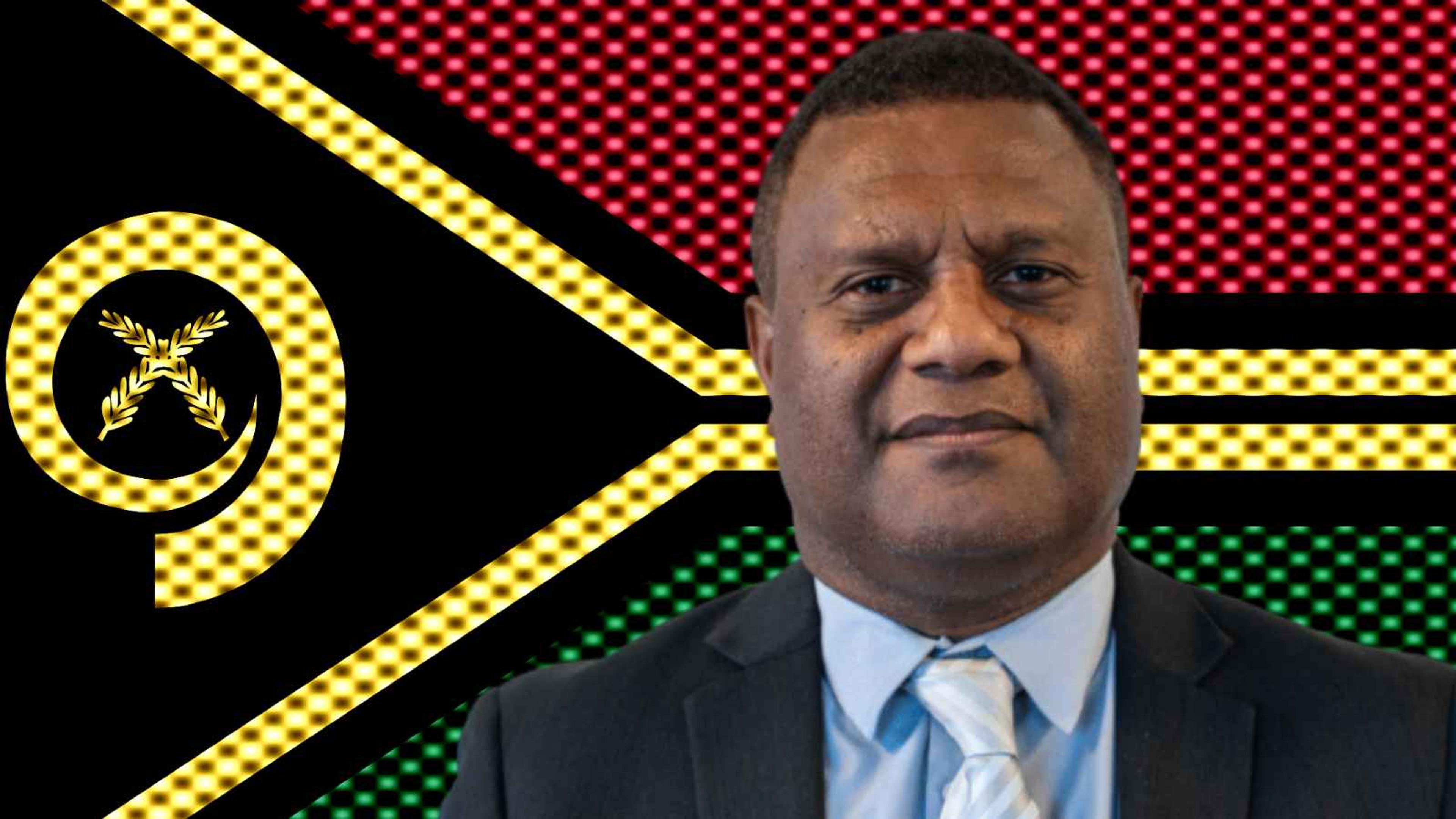
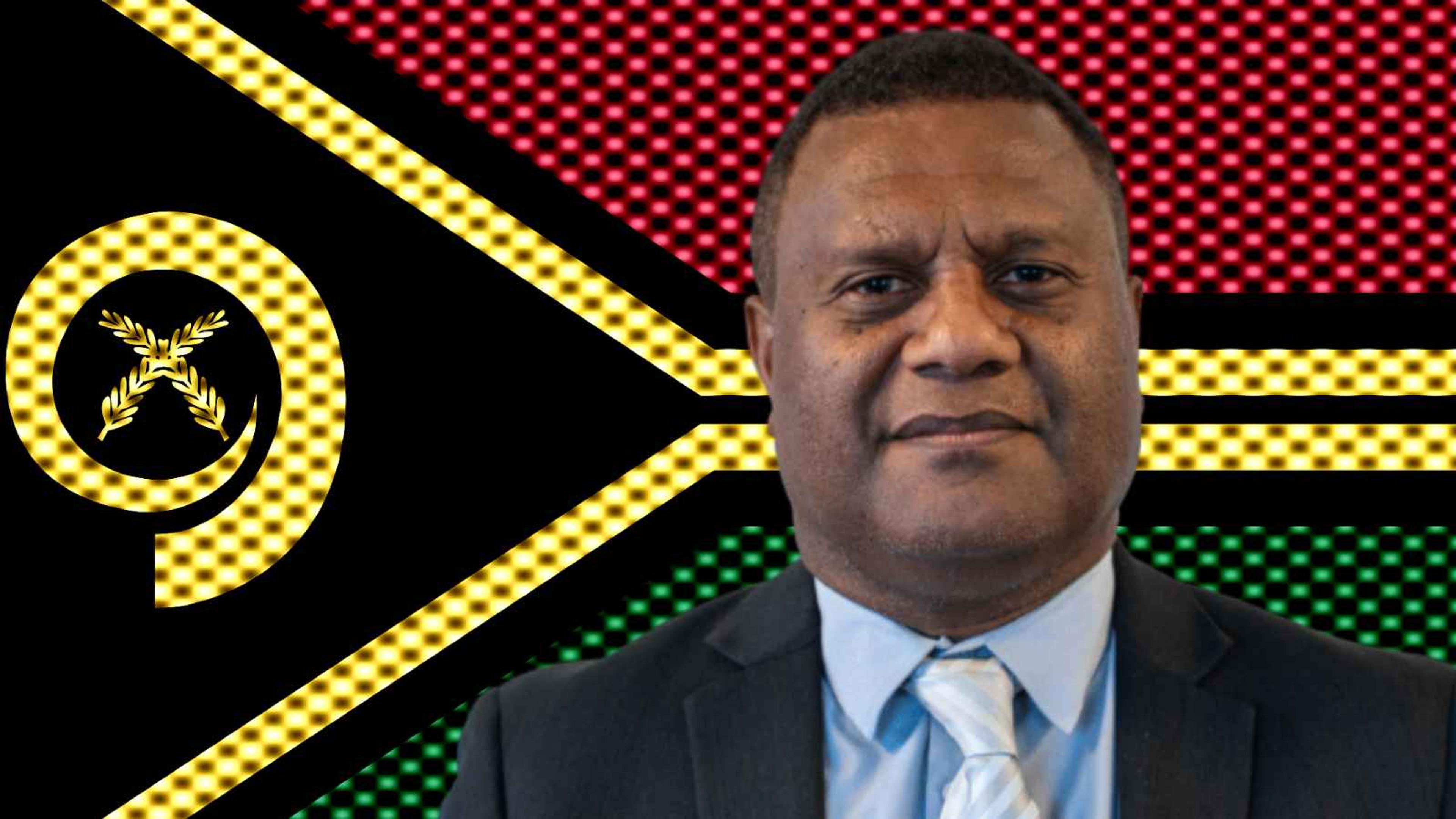
Colin Tukuitonga.
Photo/University of Auckland/Unsplash
12-month prescriptions roll out in NZ but experts urge caution for Pasifika communities
While the change aims to reduce costs and improve access, Pacific health leaders say caution is needed to ensure the reform benefits communities without creating unintended risks.

Blacklisting squeeze hits Vanuatu families and businesses, the regulator VFSC warns


Pack your tissues: Free movies return with Tinā set for South Auckland

Manurewa charity requests $30,000 to keep Pacific seniors monthly gatherings
Blacklisting squeeze hits Vanuatu families and businesses, the regulator VFSC warns


Pack your tissues: Free movies return with Tinā set for South Auckland
Since the weekend, New Zealanders with stable, long-term conditions can receive prescriptions covering up to 12 months.
The change, which came into effect on Sunday, is designed to reduce costs and improve access.
But Pacific health experts say caution is needed to ensure the reform benefits communities without creating unintended risks.
The policy allows doctors to write a 12-month prescription but patients will still collect medicine in three-month quantities from pharmacies.
This means regular visits remain necessary.
In a press release, Health Minister Simeon Brown said the approach would reduce the burden on GPs while helping patients manage chronic conditions such as asthma, diabetes, epilepsy, and high blood pressure.

Patients with stable, chronic health issues are now eligible for 12-month prescriptions as of yesterday, provided they have their doctor's approval. Photo/Unsplash
Brown called the reform a “common sense change”, saying it “will make a meaningful difference for patients with stable, long-term conditions”.
“It also reduces the time GPs and other prescribers need to spend renewing routine prescriptions, making it easier for other patients to get an appointment when they need one,” he says. “This is a win-win for both patients and health professionals.”
Speaking with William Terite on Pacific Mornings, Sir Colin Tukuitonga, the Associate Dean Pacific at the University of Auckland, welcomed th change as a potential win for Pacific families facing high medication costs but flagged some risks.
“We know that there's a lot of waste medication that people pick up, take home, put in the bathroom cupboard, and never get taken,” Tukuitonga says. “So potentially, this could increase wastage..
“But of course, one imagines that the doctors and their nurses will monitor these developments with their patients. So overall, it’s potentially a very good thing in terms of savings for people, both in money [and] time to get the script organised.”
Tukuitonga also highlighted possible economic consequences for pharmacies, saying the change could reduce foot traffic and revenue.

Sir Colin Tukuitonga, the Associate Dean Pacific at the University of Auckland, points out that pharmacies often depend on shoppers who visit for more than just prescriptions. Photo/Unsplash
Coupled with Finance Minister Nicola Willis’ warning of a tight 2026 Budget, Tukuitonga said more pressure could fall on an already strained health system.
In a press release, Gemma Perry, an independent pharmacist in Te Awamutu, said the three-month dispensing limit will maintain some contact with patients but flagged concerns over safety and professional workload.
“Many of the checks and balances people assume happen automatically are not funded,” Perry says. “They rely on professional goodwill. It’s important we don’t pretend pharmacy can simply absorb more responsibility without support.
“Pharmacists will continue working closely with GPs, but this is a complex change and it will take time for patients, doctors and pharmacies to navigate.”