

UNAIDS Pacific Adviser Renata Ram says the time for action in Fiji's HIV crisis is now.
Photo/FNU
UNAIDS official calls for urgent action, response to saving lives in Fiji
As new infection patterns emerge, driven by injecting drug use, Renata Ram urges innovative-testing solutions and harm-reducing programmes.



Niuean designers make historic debut at New Zealand Fashion Week

Siua Ikale’o: A Tongan talent’s rise to stardom in Chief of War series

Flying Fijians prove their championship status with dominant win over 'Ikale Tahi


Car audio crews fight back against govt's boy-racer crackdown

Niuean designers make historic debut at New Zealand Fashion Week

Siua Ikale’o: A Tongan talent’s rise to stardom in Chief of War series

Flying Fijians prove their championship status with dominant win over 'Ikale Tahi
The United Nations’ programme on HIV/AIDS has issued a warning about a deepening crisis that could result from a lack of bold and swift action in the fight against the disease.
As one of the fastest-growing HIV epidemics in the world unfolds, UNAIDS is urging decisive measures over the next six to 12 months to prevent this crisis from worsening.
Renata Ram, the UNAIDS Pacific Adviser, says Fiji’s declaration of a national HIV outbreak in January marks a pivotal turning point in its response to the epidemic.
“Since then, we've seen swift and serious action,” Ram tells PMN News, highlighting the establishment of a dedicated HIV and Sexual Reproductive Health Unit and the allocation of a budget that has increased from F$500,000 (NZ$370,540) to F$10 million (NZ$7.41m).
Despite these advancements, Ram says Fiji’s national HIV programme lags 20 years behind what is considered a strong, modern HIV response.
She says this places Fiji in a dual predicament: managing the current outbreak while working to improve an outdated system.
“This is very challenging, however, for the next six to 12 months, Fiji must take swift action to improve the testing turnaround time and get people to have the same-day initiation of HIV treatment.
“Also, Fiji needs to introduce the needle and syringe programme (NSP) and introduce PrEP, pre-exposure prophylaxis for HIV prevention.”
Injectable drug use is one of the key factors driving the HIV outbreak in Fiji.

Drug use is driving the HIV surge in Fiji. Photo/Google
Preliminary data for 2024 reveal that nearly 50 per cent of new HIV infections among those on antiretroviral therapy (ART) are linked to needle sharing. This marks a dramatic shift in transmission patterns, moving away from predominantly sexual transmission.
While stigma and policy hesitancy have traditionally hindered harm reduction services, Ram says that progress is finally being made.
There is now Cabinet-level support for these initiatives, and a national implementation plan for NSPs is in development, with the first national consultation held just last week.
“So, it's not a matter of if, it's a matter of when,” Ram says.
“While there's a lot of hesitancy, there is a strong political push to have this very important intervention, especially for people who are using drugs, to be introduced in Fiji, and this is going to save so many lives.”
UN data shows that only 36 per cent of people living with HIV in Fiji know their status, mainly due to stigma, a lack of awareness, and limited access to testing, especially outside major urban areas. As it stands, there are only three specialised HIV hubs in the country.
Less than 50 per cent of those living with HIV in Fiji know their status Photo/Google
“UNAIDS is really pushing for decentralised testing, more community-based testing, and also in the future to have self-testing introduced into Fiji to address these gaps,” Ram says.
“We can’t win this fight if people can’t even find out if they’re positive.”
Fiji’s situation is now viewed as a cautionary tale and a wake-up call for other Pacific nations.
Countries that once reported zero to 10 cases are now facing similar vulnerabilities, including under-resourced health systems, rising drug use, low condom use, and entrenched stigma.
“We need to learn from Fiji's example and nip things in the bud,” Ram says.
“And what we see here in Fiji could easily mirror what might unfold in other Pacific Island countries if no urgent investment in HIV prevention and strengthening the HIV programmes is made.”
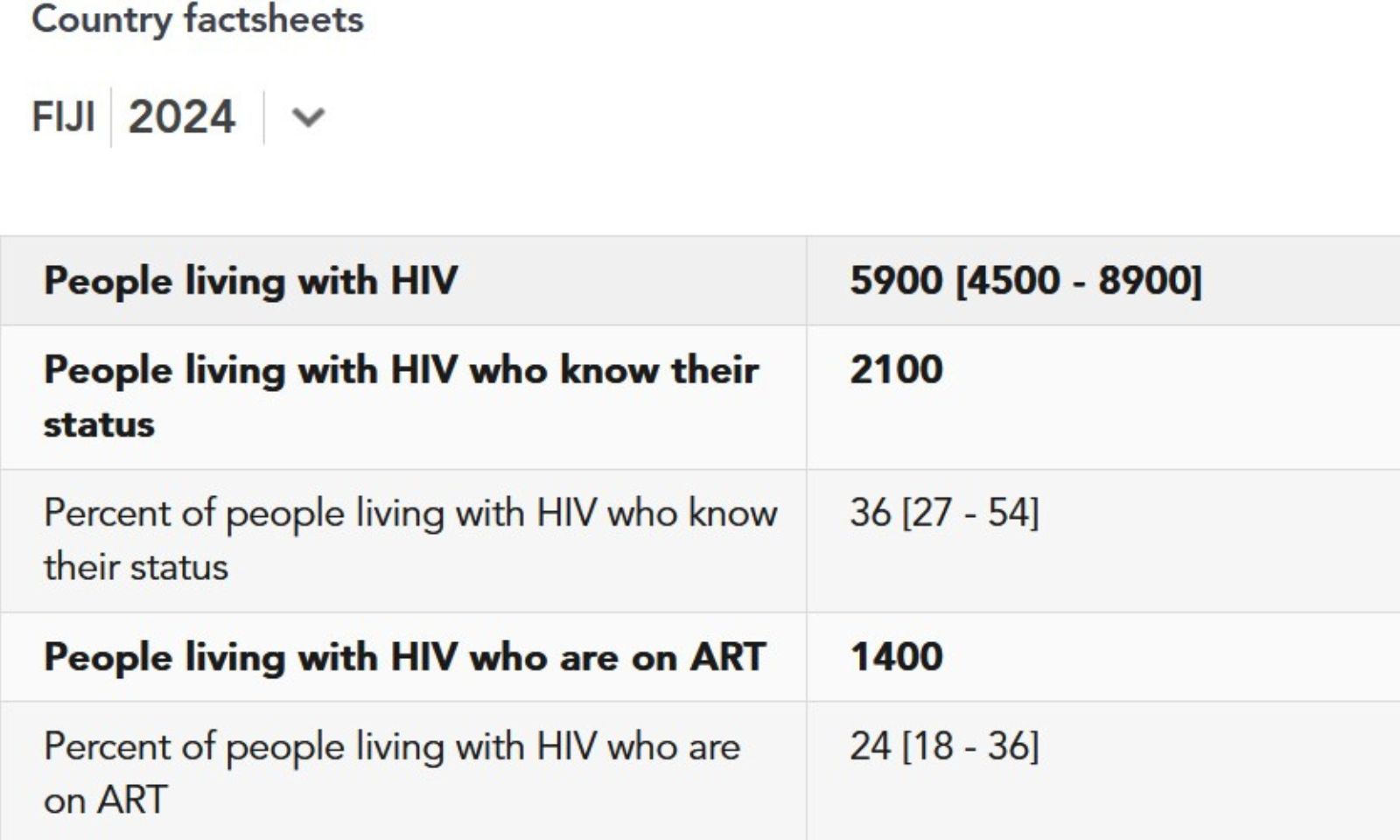
2024 HIV data on Fiji sourced from UNAIDS. Photo/UNAIDS
While donor support is growing - Australia has committed $2.5 million and New Zealand $4 million - Ram warns that Pacific Island nations still remain severely underfunded, given the scale of the risk.
“Currently, only the Global Fund is supporting HIV programmes in the larger Pacific Island countries,” she says.
“But more is still needed for the other Pacific Island countries to actually strengthen their HIV programs and have stronger HIV interventions.
“Right now, the focus is on Fiji, but we must remember that no Pacific Island country is safe unless we all are safe.”
According to Ram, success for Fiji in the next two to three years will be marked by a reversal of the upward trend in meeting the “95-95-95” target: 95 per cent of people living with HIV knowing their status, 95 per cent of those diagnosed receiving antiretroviral therapy (ART), and 95 per cent of those on ART achieving viral suppression by 2025.

Fiji's HIV Outbreak Reponse Plan. Photo/MOH Fiji
“And also building a decentralised and stigma-free system that ensures that no one is left behind,” she says. “It also means, more importantly, a model for the Pacific and a great example of how a country turned a crisis into a catalyst for transformation.”
Fiji’s Minister for Health and Medical Services, Dr Ratu Antonio Lalabalavu, estimates that 7000 people are currently living with HIV in the country.
“The ongoing upward trend is deeply concerning,” he says. “We must break the stigma and follow communities with accurate information and stop discrimination to ensure that everyone, regardless of background, has access to prevention, care and treatment.”
Lalabalavu says the HIV/AIDS outbreak in Fiji is no longer just a health issue. It is also a social and human rights issue.
“I am asking all of us…to work together and act now before it is too late,” he says. “Do not discriminate against those with HIV infections, but help them and support them to get the care that they direly need so that they can continue to be productive members of our community.”
Watch Renata Ram's full interview with The Fiji Times below.